
FAQ - Radiologic Procedure Issues
Radiologic Procedure Issues
- Which medications should be discontinued prior to an invasive radiologic procedure?
- Which procedures require that patients have coagulation studies drawn prior to the procedure? Coagulation labs include platelets, PT/INR. (PTT is no longer required for pre-procedural evaluation).
- What coagulation cutoff parameters do you use for invasive radiological procedures?
- What are the guidelines regarding barium enemas following incomplete colonoscopies?
- What formulations do you use for intra-articular steroid injections?
Which medications should be discontinued prior to an invasive radiologic procedure?
- While it is generally recommended that patients should stop taking Coumadin 5 days prior to any such procedure, it is up to the referring providers to decide when the patients should go off their Coumadin, as different patients will normalize their INR at different rates. For such patients, coagulation labs would need to be checked either the day before the procedure or day of the procedure. If labs do not meet standardized threshold criteria, the procedure may be canceled or postponed.
- EXCEPTION: Patients scheduled for arthrograms may continue their Coumadin regimen, but the procedure will be rescheduled or canceled if their INR level is above 3.5.
- Low molecular weight heparin should not be administered less than 24 hours prior to the procedure.
- For core biopsies only, patients should also stop the following 5 days prior: aspirin, non-steroidal anti-inflammatory drugs (NSAIDs), Plavix, garlic pills, and ginkgo supplements. Thyroid fine needle aspirations and all non-biopsy procedures are exempt from this last condition.
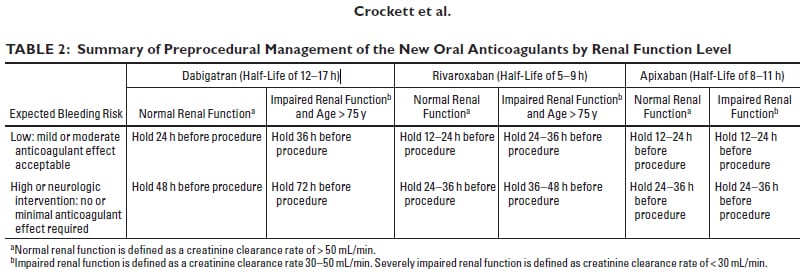
Recommendations for new oral anticoagulants Pradaxa (Dabigatran), Xarelto (Rivaroxaban), and Eliquis (Apixaban):
Which procedures require that patients have coagulation studies drawn prior to the procedure?
Coagulation labs include platelets, PT/INR. (PTT is no longer required for pre-procedural evaluation). Labs should be drawn 30 days in advance for outpatients and during the current hospital admission for inpatients.
- Angiograms
- Angioplasty
- Arteriovenous fistulogram
- Biliary drain
- Biopsies
- Central line placement (permanent or temporary)
- Cholangiograms (percutaneous)
- Cryoplasty
- Dialysis catheter placement (permanent or temporary)
- Drains and chest tubes
- Embolization and chemo-embolization
- Epidural steroid injection
- IVC filters
- Kyphoplasty
- Lumbar puncture
- Myelogram
- Nephrostomy
- Nerve root block
- Paracentesis
- PICC placement
- Pyelogram (antegrade)
- Radiofrequency ablation
- Thoracentesis
- Ureteral stents
- Vascular stents and stent-grafts
- Venograms
- Vertebroplasty
Note: Coagulation studies are only required for arthrograms, including sacroiliac joint injections if the patient is on anticoagulants.
What coagulation cutoff parameters do you use for invasive radiological procedures?
Laboratory Parameters (from: Consensus Guidelines for Periprocedural Management of Coagulation Status and Hemostasis Risk in Percutaneous Image-guided Interventions, J Vasc Interv Radiol 2009; 20:S240-S249)
These parameters are the minimum threshold for procedures and what clinicians will use as expected baselines. Individual radiologists performing the procedure may raise the thresholds on a case by case basis.
- Low Bleeding Risk: Dialysis access, venography, central line removal, IVC filter placement, PICC line, drainage catheter exchange (biliary, nephrostomy, abscess, thoracentesis, paracentesis, superficial aspiration (thyroid, lymph node, abscess):
- INR >2.0: consider correction
- Platlets if <50K, transfuse
- Do not withhold Plavix, ASA
- LMWH: hold one day prior to procedure
- Moderate Bleeding Risk: Arterial and venous intervention, chemoembolization, UFE, TJ liver bx, tunnel catheter, port, intraabdominal, chest wall or retroperitoneal bx, lung bx, transabdominal liver bx, cholecystostomy, G-tube, spine (vert/kyphoplasty, LP, epidural, facet block)
- INR >1.5: correct
- Platlets if <50K, transfuse
- Hold Plavix one day prior to procedure
- Consider correcting Activated PTT if >1.5 times normal
- High Bleeding Risk: TIPS, renal bx, biliary interventions (new tract), nephrostomy tubes
- INR >1.5: correct
- Platlets if <50K, transfuse
- Hold Plavix, ASA 5 days prior to procedure
- Hold Fractionated heparin 24 hours prior to procedure
- Correct Activated PTT if >1.5 times normal
What are the guidelines regarding barium enemas following incomplete colonoscopies?
- For barium enemas ordered following an incomplete colonoscopy, the patient should have the enema scheduled at 7-10 days after colonoscopy if any biopsy, polypectomy, fulguration, or laser coagulation has been performed during the colonoscopy.
- Otherwise, an attempt will be made to perform the barium the same day of the colonoscopy. Of note, enemas may be too difficult to perform in some patients with excessive retained gas after colonoscopy. The patients may be requested to return on the following day for the barium enema.
- Personal communication, University of WA gastrointestinal imaging staff
What formulations do you use for intra-articular steroid injections?
|
Joint |
Approach |
Technique |
Joint volume |
Kenalog 40 mg/ml |
Ropivacaine 0.5% |
|
Hip |
Anterolateral |
Fluoro |
4 cc |
1 cc |
3 cc |
|
Knee |
Subpatella |
Fluoro |
7 cc |
2 cc |
5 cc |
|
Ankle |
Anterior |
Fluoro |
3 cc |
1 cc |
2 cc |
|
Post subtalar |
Lateral |
CT/fluoro |
3 cc |
1 cc |
2 cc |
|
SI joint |
Posterior |
CT/fluoro |
1.5 cc |
0.5 cc |
1 cc |
|
Shoulder |
Anterior |
Fluoro |
4 cc |
1 cc |
3 cc |
|
Elbow |
Lateral |
Fluoro |
4 cc |
1 cc |
3 cc |
|
Wrist |
Posterior |
Fluoro |
1.5 cc |
0.5 cc |
1 cc |
|
Subdeltoid bursa |
Anterior |
US |
2 cc |
1 cc |
1 cc |
|
Tendon sheaths |
US |
1.5 cc |
0.5 cc |
1 cc |
